
Planning Your Recovery
How Opioids Change
Your Brain
It's not your fault - addiction is a disease
Opioid addiction, also known as Opioid Use Disorder (OUD) is a medical condition. It chemically changes the brain to feel “rewarded” after using opioids. Even if you want to stop, overcoming the addiction can seem impossible because of how opioids change your brain—but long-acting treatment may help.

Opioids hijack your brain
It's not your fault. Opioid addiction is a chronic brain disease. Opioid use triggers the brain's dopamine response, creating a surge of pleasure. Over time, things that were enjoyable "natural rewards" can't compete with the effects of opioids. The desire to experience pleasure or feel "normal" becomes a powerful driver to take opioids again and again.
This process impacts brain regions that oversee reward, decision-making, self-control, and learning. Together, all of these changes can make quitting seem out of a person's control.

Taking medication can help address the changes to your brain
Medication to address changes in brain chemistry may enable you to focus on counseling to establish healthier behaviors and make other lifestyle changes. While medication helps to rebalance your brain, you're able to focus on making other positive behavior changes to support your recovery journey.
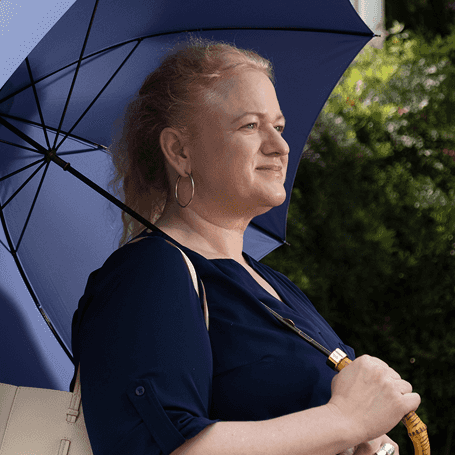
Meet Jamie. Her goal for recovery was to get back to herself.
I know the role of medication is helping me rebalance my brain so I can focus on counseling…creating healthier habits.
- Jamie
Jamie was paid by Indivior. Her story reflects her personal experience while taking SUBLOCADE.

Thinking about taking the next step with once-monthly SUBLOCADE?
Enter your ZIP code to find a SUBLOCADE treatment provider near you.
INDICATION
Prescription SUBLOCADE, with counseling and psychosocial support, is for adults with moderate to severe opioid addiction who have started treatment with a dose of oral buprenorphine or are being treated with buprenorphine.
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about SUBLOCADE?
- Because of serious risk of potential harm or death from self-injecting SUBLOCADE into a vein (intravenously), it is only available through a restricted program called the SUBLOCADE REMS Program.
- SUBLOCADE is not available in retail pharmacies.
- Your SUBLOCADE injection will only be given to you by a certified healthcare provider.
- SUBLOCADE contains a medicine called buprenorphine which is an opioid that can cause serious and life‑threatening breathing problems, especially if you take or use certain other medicines or drugs.
- Talk to your healthcare provider about naloxone, which is a medicine that is available to patients for emergency treatment of an opioid overdose. If naloxone is given, call 911 or get emergency medical help right away to treat overdose or accidental use of an opioid.
- SUBLOCADE may cause serious and life-threatening breathing problems. Get emergency help right away if you: feel faint, dizzy, confused, sleepy or uncoordinated, have blurred vision or slurred speech, are breathing slower than normal or cannot think well or clearly.
- Do not take SUBLOCADE with certain medicines. Taking SUBLOCADE with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, decreased awareness, breathing problems, coma, and death.
- In an emergency, have family members tell emergency department staff that you are physically dependent on an opioid and are being treated with SUBLOCADE.
- You may have detectable levels of SUBLOCADE in your body for several months after stopping treatment with SUBLOCADE.
Who should not receive SUBLOCADE?
Do not receive SUBLOCADE if you are allergic to buprenorphine or any ingredient in the prefilled syringe (delivery system: a biodegradable 50:50 poly(DL-lactide-co-glycolide) polymer and a biocompatible solvent, N-methyl-2-pyrrolidone (NMP)).
Before starting SUBLOCADE, tell your healthcare provider about all of your medical conditions, including if you have: trouble breathing or lung problems, a curve in your spine that affects your breathing, Addison's disease, an enlarged prostate, problems urinating, liver, kidney, gallbladder or mental health problems, alcoholism, head injury or brain problem, adrenal or thyroid gland problems.
Tell your healthcare provider if you are pregnant or breastfeeding or plan to become pregnant or breastfeed:
- If you receive SUBLOCADE while pregnant, your baby may have symptoms of opioid withdrawal at birth that could be life-threatening if not recognized and treated. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- SUBLOCADE can pass into your breast milk and harm your baby. Talk to your healthcare provider about the best way to feed your baby during treatment with SUBLOCADE. Monitor your baby for increased drowsiness and breathing problems if you breastfeed during treatment with SUBLOCADE.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements before starting any new medicines and during or after stopping treatment with SUBLOCADE.
What should I avoid while being treated with SUBLOCADE?
- Do not drive, operate heavy machinery, or perform any other dangerous activities until you know how SUBLOCADE affects you. SUBLOCADE can make you sleepy, dizzy, or lightheaded, especially in the first few days after your injection and when your dose is changed.
- Do not drink alcohol or take prescription or over-the-counter medicines that contain alcohol during treatment with SUBLOCADE, because this can lead to loss of consciousness or even death.
What are the possible side effects of SUBLOCADE? SUBLOCADE can cause serious side effects, including:
- Trouble breathing. Taking SUBLOCADE with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants can cause breathing problems that can lead to coma and death.
- Sleepiness, dizziness, and problems with coordination.
- Physical dependence or abuse.
- Liver problems. Call your healthcare provider right away if you notice any of these symptoms: your skin or the white part of your eyes turns yellow (jaundice), dark or "tea‐colored" urine, light colored stools (bowel movements), loss of appetite, pain, aching, or tenderness on the right side of your stomach area, or nausea.
Your healthcare provider should do blood tests to check your liver before you start and during treatment with SUBLOCADE.
- Allergic reaction. You may have rash, hives, itching, swelling of your face, wheezing, light‑headedness, feeling faint or loss of consciousness. Call your healthcare provider or get emergency help right away.
- Opioid withdrawal. Call your healthcare provider right away if you get any of these symptoms: shaking, sweating more than normal, feeling hot or cold more than normal, runny nose, watery eyes, goose bumps, diarrhea, vomiting, or muscle aches.
- Decrease in blood pressure. You may feel dizzy when you get up from sitting or lying down.
The most common side effects of SUBLOCADE include: constipation, headache, nausea, injection site itching, vomiting, increase in liver enzymes, tiredness, or injection site pain.
SUBLOCADE may affect fertility in males and females. Talk to your healthcare provider if this is a concern for you.
These are not all the possible side effects. Call your healthcare provider for medical advice about side effects.
To report a pregnancy or side effects associated with taking SUBLOCADE or any safety‑related information, product complaint, request for medical information, or product query contact PatientSafetyNA@indivior.com or 1‑877‑782‑6966. You are encouraged to report negative side effects of drugs to the FDA. Visit www.fda.gov/medwatch or call 1‑800‑FDA‑1088.
See full Prescribing Information, including Boxed Warning, and Medication Guide. For REMS information visit www.sublocadeREMS.com.